This is a question we often see discussed, but I think some of those discussions miss an important issue which I’m going to explore here.
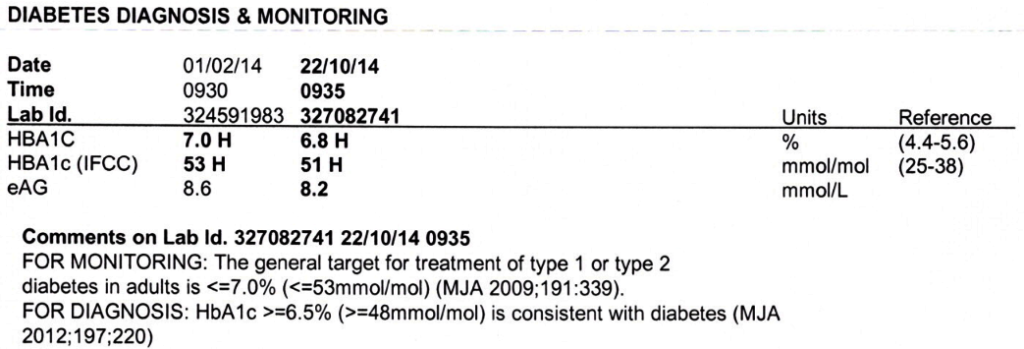
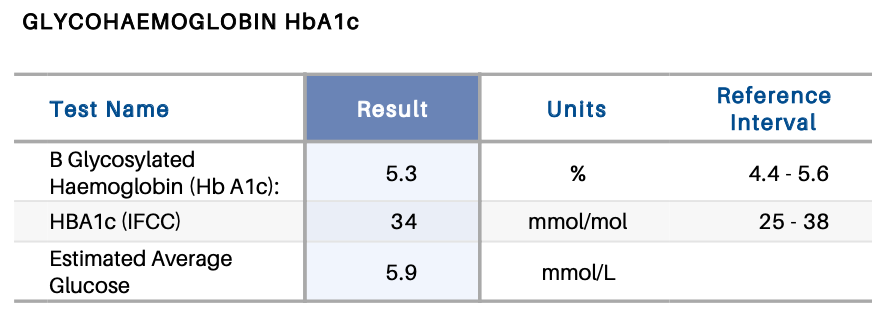
The HbA1c blood test shows us how much of the haemoglobin in our blood has been “glycated” (bonded with glucose). We’re often shown that value in the context of trying to indicate what our average BG levels have been over the preceding months. For example the estimated Average Glucose (eAG) in the above example. But it turns out that this is looking at the situation backwards.
HbA1c has an advantage in that it can be an ad-hoc test, and doesn’t need a lot of infrastructure. But its correlation with BG level can be a little approximate.
Actually measuring our average BG level requires good CGM to get accurate results (or many fingerpricks per day including while asleep), and many people do not have access to that (for example most Australians with T2D, as well as many people with T1D elsewhere in the world).
So which should we use? Let’s explore what the HbA1c test is actually measuring.
Glycation
The average person apparently has haemoglobin which lasts for about somewhere between 105-117 days before it’s recycled by the body. It’s continually replaced by new haemoglobin being generated by bone marrow. During its lifetime, as it’s exposed to glucose in the bloodstream some of it bonds with the glucose (becomes “glycated”).
So by looking at how much is glycated, an extrapolation is often made as to what our average BG has been. However there are a few factors that this calculation depends upon. At least these three:
1. Changes in the blood glucose levels
Due to the gradual replacement of the blood cells, a sample now will contain more cells from last week than it will from 100 days ago. If our BG patterns have been consistently higher over the last weeks/months then it’s likely the HbA1c will be higher. And vice versa: if our BG patterns have been dropping, the recent data will have more impact on the HbA1c. We would expect to show a lower result than a simple arithmetic mean of the last 3 months’ BG numbers would indicate.
This difference is usually not significant, but it’s still there. In some cases it could account for HbA1c variations of at least 0.2-0.3%. Although mathematically the most recent month contributes about half the value it’s uncommon to have a sudden huge variation, and it’s a gradual shift in significance over time.
2. The lifespan of the haemoglobin
The average may be 106 days in women and 117 in men, but not everyone has that. In fact some people have red blood cells which are recycled much faster. So older BG levels may have even less impact on the HbA1c result. And issues such as significant iron deficiency can extend the lifespan.
Blood loss (e.g. through donation) followed by accelerated replacement with young haemoglobin can obviously have impact too. See “Whole Blood Donation Affects the Interpretation of Hemoglobin A1c“.
3. The glycation rate
When exposed to the same BG level, not everyone’s haemoglobin will be affected at the same rate. It might take one person more time for the haemoglobin to become glycated than another. This person would probably end up with a lower HbA1c result.
Can we reliably map between HbA1c and BG?
There are presumably more factors than just those, but I think they’re likely to be the major ones in most cases. It’s unfortunately not a simple mapping of HbA1c to average BG in all cases. Consider the graphs we looked at in “GMI and HbA1c revisited” such as this one:
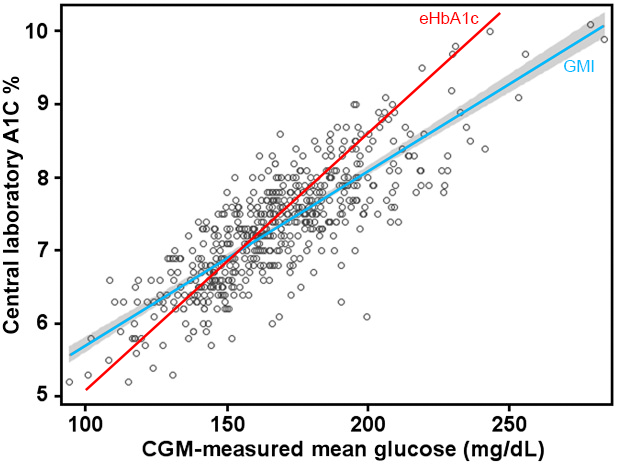
Those dots are the data set that was used to generate the GMI formula via linear regression. The earlier eHbA1c formula was generated via a similar mechanism from an earlier dataset.
There’s a vague association for this cohort of samples, but many of them don’t closely follow the red or blue lines. As you can see, at around 170 mg/dL (9.4 mmol/L) some people got HbA1c values around 6%, while some got over 8.5%.
Meanwhile at that point the GMI formula gives 7.4% while eHbA1c gives 7.5%. Inverting those formulas on either 6% or 8.5% will give wildly different estimates of the average BG.
Ask the right question
But it’s not a question of “which one is right?”, it should be a question of “why did those people get those results?”
We already know that variations in BG level over time and the lifespan of the haemoglobin can have effects. In fact in the GMI study referenced above those mean glucose numbers were generated from samples of just 14 days (just the last 2 weeks, not the last 15+ weeks).
But a big factor seems to be the glycation rate. Maybe some people “glycate faster” and get higher HbA1c values. In fact there’s been some work done on modelling this and using a glycation factor in the conversion.
It’s probably a mistake to just take away from that the conclusion that those people need a different calculation to come up with the BG number.
It may actually be more important to look at the HbA1c number itself.
Extrapolating BG from HbA1c
This shouldn’t be news to anyone, but it’s worth repeating. HbA1c is often used as an indicator of the average BG levels over the preceding months (although it runs into problems with some physiologies) but it doesn’t say anything about the highs and the lows (the “rollercoaster” we’ve been on) which are known to be clinically important. It’s “averaged” everything down to a single number, and it’s “too averaged” for many uses.
It doesn’t directly indicate anything about our exposure to hypo events for example.
Where HbA1c can be useful though is for those people who do not have access to CGM data. It should be better than nothing as a guide, but unless we know if that person is a “high or low glycator” the result can be untrustworthy.
But do we need to know the average BG?
Our instantaneous blood glucose is something we can see when we do a fingerprick meter test. It’s a thing we can see and often we can act on directly (via food, exercise, medication, etc).
We’re told that keeping our glucose at a reasonable level is important, and measures like Time In Range can help us target our management to achieve that. But is that enough?
All we can really say is that keeping our BG “in range” will reduce our risk of developing health complications. But there are no guarantees.
There are people who have maintained optimal BG levels but still eventually develop “diabetic health complications”. And there are people who have had BG levels ranging all over the place for years and yet seem unscathed. The simple answer sometimes given is that it’s essentially a “genetic lottery”. Not knowing your lottery result before it hits you is hard.
Yes trying to keep our BG levels under control is very important. But unfortunately it’s obviously not the whole story.
So is HbA1c useful?
It does show us how much of our blood has become glycated. It is constrained by issues such as haemoglobin lifespan, but it seems reasonable to treat it as an indicator of how much glycation we’ve been exposed to. So yes it has some direct value.
Glycation again
The glycated blood cells can be a problem of themselves. The cell membranes are affected, and this can lead to cell aggregation and increased blood viscosity. It can also increase inflammation, and this has been linked to damage to other cells in the body as well as increased risk of atherosclerosis (e.g. plaque in blood vessels). In fact, there are theories that the glucose may also glycate LDL cholesterol directly, further contributing to sdLDL particles and plaque formation. Either via indirect effects via the haemoglobin or via direct glycation of other cells, we don’t want too much glycation going on.
Some level of glycation is normal and healthy. Glucose is a major fuel source for some parts of the body, and needs to be transported around the body. But it’s generally accepted that too much glycation along the way is bad.
A flow-on from this is that the HbA1c result may directly indicate the glycation risk to the whole body.
It indirectly indicates the average BG level, but maybe that’s not the primary role of this measurement.
Can we get rid of HbA1c already?
I’m not sure we can.
It definitely should not be used as a judgement of whether we’ve been “good” or “bad”.
We do our best to manage our BG levels as that’s what we have visibility of and some hope of direct control over, but BG is not the only factor contributing to HbA1c.
Glucose levels are a big factor in HbA1c, and they’re also important in that if we don’t have the right levels we can suffer other issues (such as immediate hypo effects, possible long-term cognitive issues due to frequent deep hypos, and suppression of the immune system in hyperglycaemia).
But the other factors are important too.
Unless the other factors such as glycation rate are likely to change over time, I’m not convinced that once a relationship between CGM data and HbA1c has been established that there’s a lot of value in regular HbA1c measurements if we have decent CGM coverage.
Of course if we’re having panels of other blood tests done for monitoring (which seems sensible: there are lots of mechanisms in the body which can and do change over time) then having an HbA1c test done on the same sample should introduce little hardship.
So what can I do if my HbA1c doesn’t match the predictions?
Apart from the obvious response of “discuss it with your doctor”, there seem to be some generalities we can make.
Maintaining good glucose levels is always a good idea. I would not lose sight of that as a goal and a useful tool.
If your HbA1c readings come in consistently lower than the eHbA1c or GMI predictions from your CGM software, then you and your medical team might decide to not pay those readings much attention. I’ve seen that happen. It’s essentially acknowledging that something in your body may be invalidating the HbA1c data.
If your HbA1c readings come in consistently higher than the predictions, it would be tempting to treat it in the same way. However due to the risks associated with glycation I would be exploring with my medical team everything that we can do to keep me protected in light of that. Presumably as well as managing the glucose levels this might include other things such as statins to help reduce the risks associated with lipid glycation. Managing the risks around our kidneys, eyes, etc may be even more important for people in this category than the “average” person.

Thanks for this. Always good to receive your balanced and informed analysis. Useful.
Great article.
I agree with the hba1c being a metric that may not be valid.
My number has been 4.2 for the last few years yet my CGM says I average around 5.0
Clearly my body doesn’t comply with the way the hba1c is calculated.
Thanks for all the insight here as my endo had no idea as to how to deal with my consistently low hba1c.
Good article. You give a good overview of what HbA1c measures and how it is relevant (and some of the shortcomings of relying on it).
Just one small comment: you mention glycation in relation to transporting glucose but my understanding is that glycation is essentially irreversible. Therefore, glycated haemoglobin is just carrying around useless glucose, not delivering it anywhere. Also, that is why the lifespan of haemoglobin is relevant: the glucose doesn’t become separated from the haemoglobin until is is broken down. If the glycation was reversible during the lifespan of the haemoglobin, HbA1c would probably not be much better than instantaneous blood glucose concentration in estimating long-term blood glucose levels.
Aside from affecting the viscosity of blood, glycated haemoglobin is also not as efficient at carrying oxygen (perhaps unable to, I’m not sure), which is the main function of haemoglobin. That can make our bodies less efficient and cause damage.
You’re right, glycation is not reversible.
My comment about the blood transporting glucose was meant to be in the context that some glycation is unavoidable given that the two things are in contact.