So another quarter has rolled around, and another blood test has been done. Here’s an analysis of my last 90 days of CGM data. This goes back to mid-December 2019 (so includes Christmas/NY).
Compared with lab HbA1c
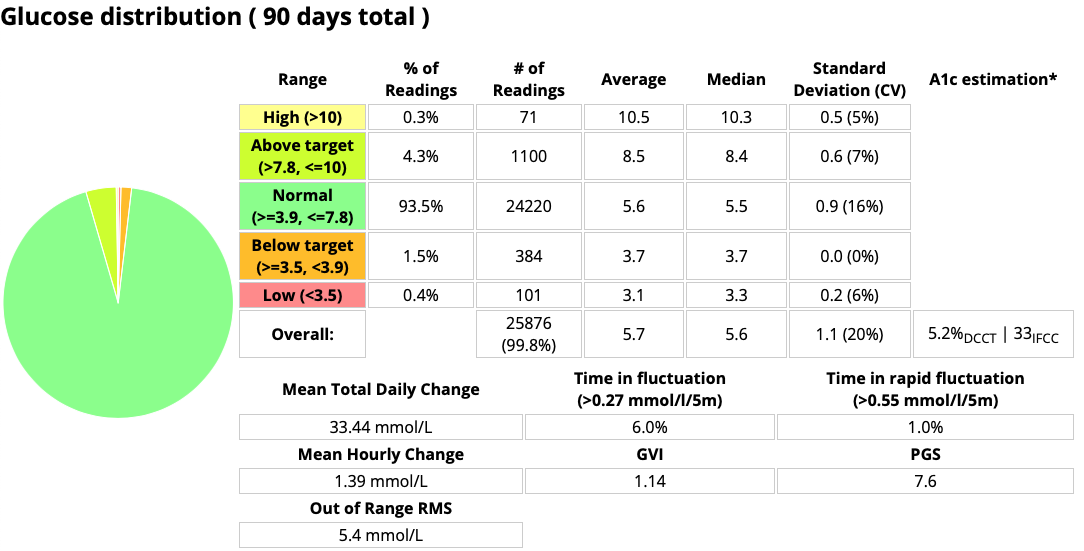
Each day is different, but the above data is an average over the last 90 days. For the last few years the A1c estimation from the CGM data has been within 2 mmol/mol (approximately 0.2%) of the lab result. Recently it’s been very close: usually exactly the same.
But this time the lab result was slightly different. 31 mmol/mol (5.0%)
I was actually expecting to see either 33 or 32 (5.1%). The above is a plain average over the last 90 days, but the actual HbA1c result is weighted towards the more recent results (due to the linear decay of the haemoglobin population over 120 days) and over the last month the CGM average has been predicting 32 (5.1%). At this point my endocrinologist reminded me that the precision of the HbA1c test is not absolute so it could be the same thing. But we were happy to take the “5%” figure as the milestone!
Highlights
The key “take-aways” from this data for me are:
- My HbA1c is smack in the middle of the “reference range” of 25-38 mmol/mol (4.4-5.6%).
- My CV (coefficient of variation) has dropped to 20%. Any decrease in this is a reduction in my variations (an increase in the “tightness of control”). I do get weeks of <18%, and it’s nice to see that creep into the longer-term average.
- My time below 3.9 mmol/mol has dropped a little since the last check. Any reduction in hypo time is a good thing!
- Green is a pretty colour…
All in all, I’m happy with the statistics of my glucose data.
Generalised T1D goals
How do these results compare with the generalised advice that’s often given out regarding T1D management in adults?
Please remember, that these are presented to us as goals.
Aspirational ones, and not necessarily easy to achieve for many people with the tools they currently have.
| Metric | Generalised Goals | David Jan-Mar 2020 |
|---|---|---|
| HbA1c | <= 48 mmol/mol (6.5%)
<= 53 mmol/mol (7.0%) for people with elevated hypo risk |
31 mmol/mol (5.0%) |
| CV | <= 30% | 20% |
| TIR for 3.9-10 | > 70% | 97.8% |
| Time below 3.9 | < 4% | 1.9% |
Smashing it! All my doctors are very happy with these results (I’m sure some of them think I’m an overachiever). I didn’t always achieve data like this, but I’ll go over that history in the next article.
How far can we go?
From EASD back in 2018 we saw a summary of CGM data gathered from 153 people without diabetes. If we take that population as an example of “normal”:
| Metric | “Normal” | David Jan-Mar 2020 |
|---|---|---|
| HbA1c | 32 mmol/mol (5.1%) | 31 mmol/mol (5.0%) |
| CV | 17% | 20% |
| TIR 3.9-10 (70-180) | 98.9% | 97.8% |
| TIR 3.9-7.8 (70-140) | 96.8% | 93.5% |
| Time below 3.9 (70) | 1.1% | 1.9% |
| Time below 3.3 (60) | 0.2% | 0.2% |
I don’t need to match the average of that study population, but yet it looks like I’m starting to get close. In fact it’s possible I’m already within the spread of their results!
I’ve recently made some changes which I’m hoping will reduce my time below 3.9 mmol/L even further, so we’ll see what happens in the coming months.

This gives me some confidence about my long-term health prospects. Despite the recent diagnosis of mild heart disease, and the knowledge that health complications can happen to all of us.
Especially in this time of the COVID-19 pandemic, having my glucose levels in such a healthy range does let me concentrate my worrying on other issues!
How am I doing this?
It used to be that I didn’t get results anything like this, but a few years ago made a bunch of changes which seem to be paying off. It’s a combination of:
- Using a closed-loop insulin pump system (I’m using AndroidAPS which ties my Dexcom G5 CGM together with my Accu-Chek Combo pump). This makes tweaks every 5 minutes, and adjusts for things even when I forget to do them (which happens all too often!).
- Diet. I don’t do “low carb” or “keto” eating, but I am quite conscious of eating healthily. I have to for my coeliac disease anyway.
My carb intake is currently about 130g/day (>1.3 g/kg of body weight) and mostly (but not completely) lower-GI choices with a reasonable mix of other nutrients.
But I have been able to decrease and increase my carb intake without unduly affecting the BG levels. I don’t design my diet around “X carbs per day” but rather as a balanced proportion of “X kilojoules per day”. - Exercise. In the last year I’ve been doing more regular exercise (mainly riding and walking) which has been helping with the overall fitness.
- Using the feedback the loop gives me, I tweak both its parameters and my behaviour.
For instance recently I had a few hypo alarms despite the system reducing my insulin. After examining the patterns in the data it seems that my insulin sensitivity had increased slightly again (presumably a combination of gradual weight loss and slightly increased exercise). So I scaled everything back by 5% and things settled down.
I’ve also learnt better ways to declare my food intake to the system to help it minimise post-meal spikes, how to manage food/insulin intake around exercise, etc.
I don’t think there’s anything particularly “magic” about this, but the closed-loop technology has definitely had a major role in enabling everything else.
CGM and modern technology can work!
I wouldn’t be able to achieve these results without CGM. Unfortunately like more than half of Australia’s T1D population I’m not covered by the Australian government CGM subsidy (including the March 2020 expansion). I have to cover the cost myself.
I’m aware that not everyone will manage to get the results I have (and in fact I know some people surpass them) but I do think this is a real-world example showing the dramatic improvements that CGM enables. I look forward to the day when these technologies are available to all people living with T1D!

I was wondering what diet your followed. I follow a “loose keto” but I don’t count calories or carbs. I just try to choose lower carb options. I avoid sugar, bread, rice and potatoes (except an occasional serving) but sugar and grains make me feel like crap even in barely detectable amounts. I’m LADA right now and not taking insulin. Just metformin so I may have to increase my carbs if I ever go on insulin which I’m told is inevitable but it could be years away too. You have great presentation skills. Good, clear visuals and supportive text. It makes me feel less worried if and when I ever have to go on insulin. The technology will probably only improve over the next few years if my pancreas holds on a little longer. LOL!