Recently I spent a day participating in a training course for endocrinology registrars (i.e. doctors). It was the Practical Skills Course for Endocrinology & General Medicine Advanced Trainees run by the Australian Diabetes Society. I’ve participated in this course for several years now. I was there as a consumer/demonstrator to help educate the attendees on things like BG monitoring (including CGMs) and insulin pumps, but I also got to sit in and listen to the training on other areas such as managing Type 2 diabetes.
One presenter was talking about target BG numbers (and associated HbA1c). In relation to T2D, but in reality the knowledge about risk profiles is primarily based off HbA1c data which applies to everyone no matter their type of diabetes. This clinician presenter made an off-hand comment which struck me. I’m paraphrasing from my notes, but essentially they said that:
“Really tight glycaemic control increases risks [such as heart attack]”
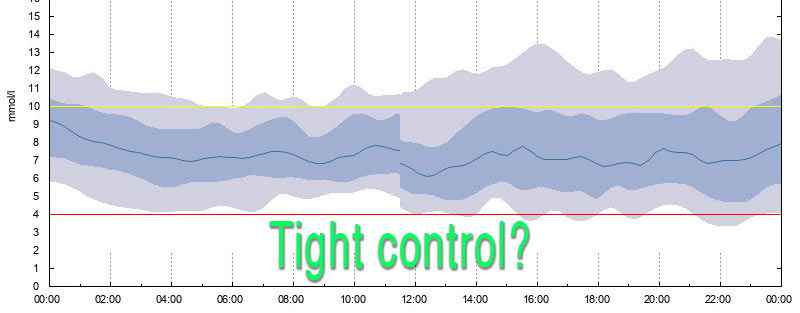
My first response to this was “No it doesn’t!” And then I realised that they were using a different definition of “tight glycaemic control” to that which occurs to many people who live with diabetes. Especially those of us who live with CGM and see our real-life BG patterns.
- To this doctor, “tight control” meant “low HbA1c”.
- To me, “tight control” means “low variability”. Keeping the numbers in range.
Sure, having tight control over my BG levels has meant that over time I’ve been able to safely lower my average BG level (and thus HbA1c). But it’s possible to have “tight control” and yet keep the numbers at a different level.
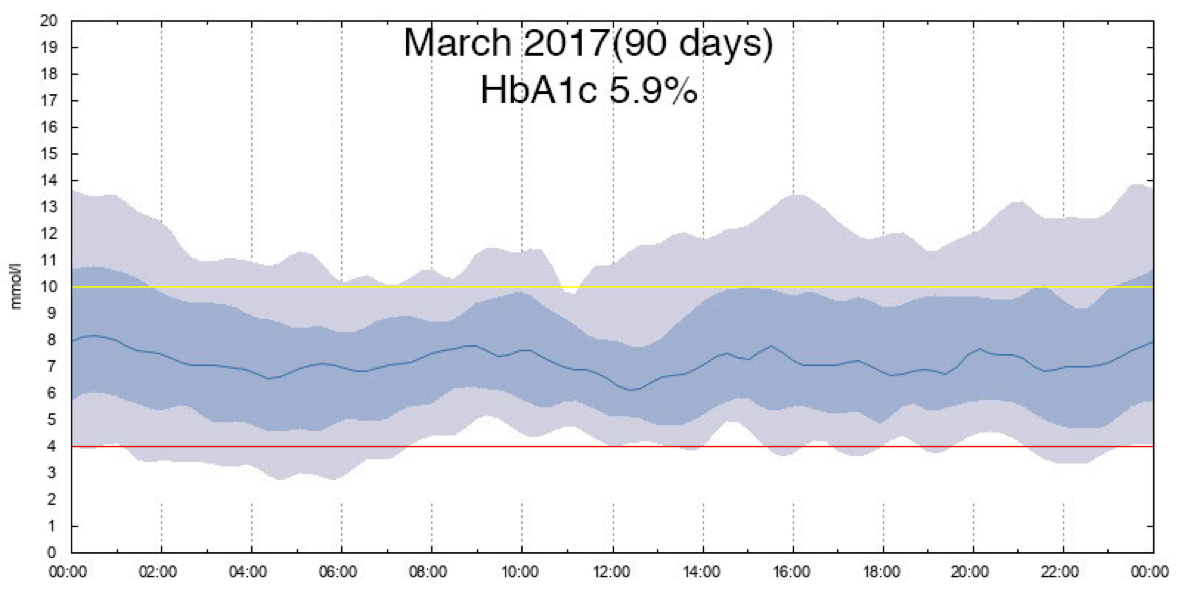
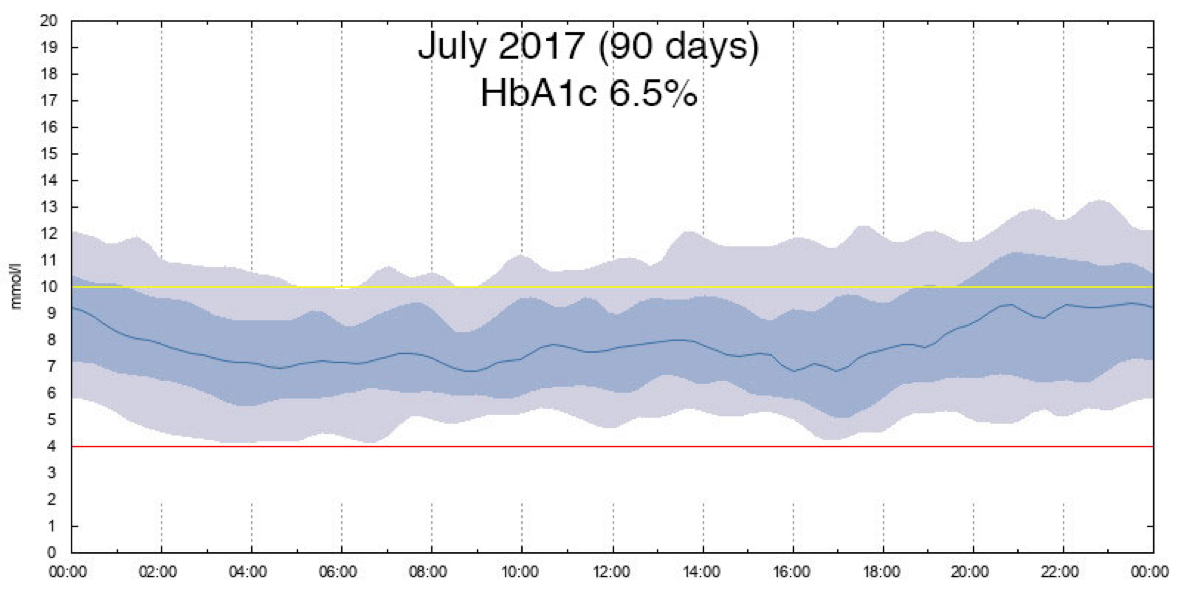
Here are two real-world examples from my own pre-looping history.
I think this is closely related to the issue I discussed last October. Aiming at a lower HbA1c is not a good way to achieve “tight control” (or even to safely achieve a lower HbA1c). Tightening up control can then allow you to achieve a lower HbA1c, but that is not the same thing.
“Tight glycaemic control” being mis-used
I queried this presenter about the topic afterwards, but they seemed to have trouble disassociating “tight control” from “low HbA1c”. In the research-driven world there have been very few studies about glycaemic variability, so it makes sense that researchers were used to often only thinking about HbA1c.
Basically I got the line of “No, tight control is the same thing as lower HbA1c. That’s what it’s always meant. Low glycaemic variability is something else.” Again that’s paraphrasing, and admittedly it was a brief conversation where we didn’t have a chance to explore the discussion much further.
I do get the feeling that many in those research and clinician communities do not have a full understanding of what “having control” really means. How many of them actually live with diabetes and experience the concept of “glycaemic control”?
Incidentally, one of the presentation slides said “The ACCORD study suggested that very tight control in people with long-duration diabetes […]”. Actually I can find no use of the word “tight” in the 2007 Action to Control Cardiovascular Risk in Diabetes (ACCORD) paper. So I have to assume the language has been added by people putting their own interpretation on the results.
However this presenter is definitely not the first person to use “tight control” in this way. There are many examples visible on the internet of researchers and doctors conflating the concepts “tight” control and “aggressive” control. Maybe that community does define “tight glycaemic control” as “achieving low BG values”. It doesn’t mean they’re not wrong to do so though!
Better language
If the presenter had simply said something like
A very low HbA1c can increase risks […]
then the issue wouldn’t have come up at all.
Especially in training material that’s being drilled into the minds of the next generation of endocrinologists!
Of course if the words “does” or “will” were used instead of “can”, that would open up a whole other argument…

Thank you David for this insightful post.
What concerns me perhaps more is when people say say, “80 % in range”. The problem is that people have different ideas on what the ‘range’ for acceptable bsls is.
Most posting on sites seem to be talking about what their pump is telling them, perhaps little realising that is likely to be the American Diabetes Association guideline for blood sugar range of (in mmol/l 3.8 to 10.
Maybe everyone ask your doctors if that range is likely to keep you from harm’s way in future.
And also ask them why such a range would have been decided on.
And what evidence is there that said range is best for diabetics (as opposed to for the doctor).
Certainly the standard clinical “range” usually used in diabetes circles is 3.9-10 mmol/L (70-180 mg/dL) although some people round that up to 4-10 mmol/L.
Yes that is a larger range than is physiologically “normal”, although it is at least a goal that provides a starting point.
If you told people they should be aiming for 3.6-7.8 (65-140) for example, that might be closer to “normal” but introduces problems such as being much closer to the clinical 3.0 “hypo” mark, as well as being much harder for people to achieve when they’re starting out. And there has to be some recognition that because we no longer have “normal” autonomous control systems in place it is harder to achieve “normal”. Even those of us with CGM need some “safety buffer” above the clinical hypo mark.
Unfortunately there is no evidence to show the effect (or lack of effect) of occasional hyperglycaemia, and only of the average BG. But 3.9-10 does seem a reasonable starting goal (which can at the same time assist people to achieve a lower HbA1c, which is where the evidence lies).
Personally, I currently measure my BG against a 3.9-7.5 (70-135) range. But getting there has been a very gradual process over a few years. If I’d aimed that tightly when I started, I would probably have floundered early. It was certainly hard to imagine such a goal early on. My earlier “Targets and Goals” discusses some of this.
A benefit for me is that when my data is instead analysed against the 3.9-10 range the numbers look even better and no doctor gets on my back. But it’s not the range I measure myself against.
If you’ve seen some of the articles where non diabetics wear cgms, you’ll see the body’s blood sugar can go up and down throughout the day.
In fact, spikes happen in non diabetics too its just their time out of “range” is significantly lower.
A good range is whatever a person is trying to achieve, its individual. Someone who might have a hba1c over 8 or 9 might be trying to achieve a range of 5-10 to avoid lows but also not overtreat highs.
Or maybe they are trying to stay in range for 75-80% of the time.
A “low” hba1c can mean more time having hypos in some people so this all needs to be taken into context.
Indeed. In fact there’s an example of “non-diabetic” CGM data in a recent post on this site. Hypos present real health risks for everyone, and a “low” HbA1c that involves too many hypos would arguably be less healthy than the same HbA1c level without so many hypos.
But judgements about what ranges and levels are appropriate for each person are quite separate from the concept of someone managing to achieve “tight control” of their levels (whatever levels those are).
The single metric available in HbA1c says nothing about how tight the control is. “Loose control” at a lower HbA1c level would probably involve more hypos than someone maintaining “tight control” at that level.