Continuous Glucose Monitoring (CGM) technology is a tool that enables a lot. Including the Automated Insulin Delivery I rely on. But it’s been very expensive.

In the lead-up to this week’s Federal Election, there has been bipartisan support for a promise to extend the current NDSS CGM Subsidy program to cover all Australians with Type 1 Diabetes.
 This is wonderful news. For our quality of life, our pockets, and for the economy and society as a whole. It’s been known for a while that the improvements in long-term health and reduced costs to the healthcare system will be massive compared to the investment in a subsidy. It’s good when we see governments doing things that should pay off in everyone’s long-term benefit and not just in votes for their next term in office!
This is wonderful news. For our quality of life, our pockets, and for the economy and society as a whole. It’s been known for a while that the improvements in long-term health and reduced costs to the healthcare system will be massive compared to the investment in a subsidy. It’s good when we see governments doing things that should pay off in everyone’s long-term benefit and not just in votes for their next term in office!
This change is probably a doubling of the current support: which essentially only covered young people, those with health concession access, and people working on (or achieving!) pregnancy. It’s still a long way from equitable access for everyone who can benefit from CGM technology (such as many people with T2 along with other types of diabetes and similar conditions) but it’s a nice step forward.
What will happen, and when?
All we know so far is a promise that the system should be available from the 1st of July 2022. And that it should involve a monthly cost of no more than $32.50. The people getting it for free under the current scheme will not be affected. But we don’t know exactly how it will work, and we’re left hoping that this election promise does turn into reality. Not all do.
We don’t even know if that $32.50 is supposed to cover sensors as well as transmitters: there are no details available yet. We don’t know how the pricing would change for someone with temporary PBS SN SafetyNet concession status (would there be a reduced price like for BG strips and pump consumables, or would we magically get them for free?). There are lots of fine details which should come to light as we get closer.
If you’re wondering what gear might be available, I can only point you to the current NDSS CGM order form:
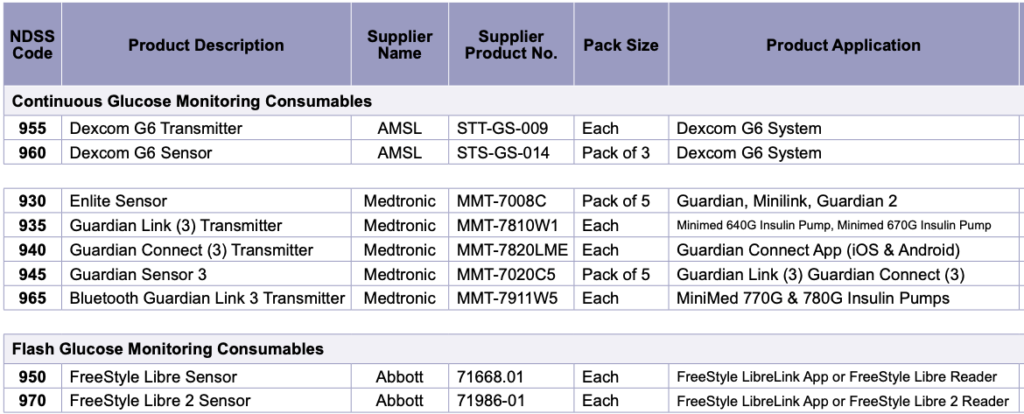
Mind you, the Libre (code 950) has already been discontinued by Abbott.
We don’t know if we will have to pre-register with the details of which CGM system we want to use (currently this needs sign-off from a clinician) or whether we will be free to pick and choose as we currently do with all our other NDSS supplies. NDSS already knows if we’re classed as having Type 1, so hopefully we don’t have to go through too much extra paperwork. I’m hoping the system will become clear during June.
Warranty support
It’s important to remember the warranty situation. This has tripped up many users of the current subsidy scheme. When we buy our CGM equipment from the companies, if they fail we don’t just write off a hundred dollars on a failed sensor. We expect to (and do) get warranty support from the company, with replacement equipment for free.
The same applies to gear supplied via NDSS. Probably influenced by the fact that it was “free” gear, some people would just throw out failed gear and then collect more from NDSS. However that hits a serious problem when you’re eventually told that you’ve hit your annual quota of equipment, and can’t get any more until the year is up. If equipment is faulty, you are expected to report it to (and get replacements from) the company directly. The fact that they sold the gear to you via NDSS is not relevant: they have to stand behind their products.
We don’t know what the NDSS quotas for CGM gear will be, but based on past experience it will probably be an annual setup with enough for the year along with a few spare boxes. But the quotas for other NDSS consumables are done on a rolling 180-day period, so we’ll see what we end up with.
But when?
If the system does go live on the 1st of July (which is a Friday) we don’t know if the pharmacy system will be swamped with orders and subsequent delays. I think it would be foolish to assume that we will be able to have new CGM sensors in our hands on the 1st. If we’re lucky some people might receive them by the 4th.
So for the people currently paying thousands of dollars per year for their CGMs and trying to work out if they have enough to get them through the remaining time to the subsidy, it would seem sensible to have a little buffer of sensors on hand to cater for delays.
I’ve already bought another box of G6 sensors to get me through to late July (my sensors are lasting me around 18 days each). Hopefully after that it should just be a case of ordering regularly through my pharmacy like I do with my other NDSS supplies.
One would presume that online ordering systems laid on top of NDSS would get extended too. MedAdvisor is one system that people use to be able to place NDSS orders via app whenever convenient, and pick them up from the pharmacy later (although they are notorious for not listing all the options available). Stripped Supply is a new enterprise which is setting up regular automatic delivery of your supplies (although for pumps it currently only supports Medtronic and Tandem users).
If and when all these systems update to include the new CGM subsidy obviously remains to be seen.
CGM subscriptions
I’m aware of statements from Dexcom and Medtronic that people with current CGM subscriptions will be able to transition to the NDSS scheme at no financial penalty. I assume that Libre is the same. But again, I would not expect the changeover to happen on July 1st!
Possibilities and predictions
So much for the obvious details of how the system might be implemented. But I think it’s also worth at this point exploring what CGM might do for you, and what the new availability might make possible in terms of opportunities for all of us!
CGM is not a “magic pill” by itself
After the NDSS CGM Subsidy was introduced for kids in 2017 and had been in place for a while, some people criticised CGM as “not being worthwhile” because there wasn’t the huge improvement in clinical results that they’d been hoping for.
It seems obvious to most of us that this can be directly blamed on the lack of education and support around CGM at the time. Many parents struggled with the systems and some stopped using them as it seemed “too hard”. And the healthcare teams supporting them were not given extra time (or funding) to guide them.
There is a risk that similar issues may hinder the uptake this time too, but hopefully some lessons have been learnt.
CGM is a powerful tool
But the configuration needs to be appropriate for your current situation. The alarms can be useful (and even sometimes life-saving) and some people set them “tight” to prompt them to make corrections (usually carb or insulin-related) and thus stay within their target range. But if you set the alarms too tight then it’s easy to end up with “alarm fatigue”, ignoring them and in fact deciding not to use the CGM at all because it’s too annoying.
 Indeed sometimes it can be helpful to have the alarm range set fairly wide, allowing us to glance at the data and make decisions without being interrupted all the time. This relates back to what I wrote in 2019 about “Targets and goals“, where I started out with a wide goal range and gradually narrowed it over time. Having a too-narrow goal range can lead to frustration when you “just keep shooting out the other side” even without considering alarms.
Indeed sometimes it can be helpful to have the alarm range set fairly wide, allowing us to glance at the data and make decisions without being interrupted all the time. This relates back to what I wrote in 2019 about “Targets and goals“, where I started out with a wide goal range and gradually narrowed it over time. Having a too-narrow goal range can lead to frustration when you “just keep shooting out the other side” even without considering alarms.
Unfortunately some of the current software insists on having alarms at the edges of the goal range you specify (I prefer to have a visual goal “band”, with alarms a little further out). But these functions may develop over time. Software like xDrip+ already has a very flexible alarm framework (I have used xDrip+ as my main CGM since 2017).
Not just alarms
Compared to fingerpricks, CGM shows us what happened while we were not looking. While we were asleep, while we were digesting a meal, and throughout the day. The Dexcom and Medtronic systems keep the history data for 5-minute increments. The Libre software averages that back to 15-minute increments, but even that can tell you a lot.
 If you’re using the Dexcom G5/G6 app as your CGM it only shows the last day’s data, but it uploads data into Dexcom’s servers, and you can use the Dexcom Clarity app on your phone or via the web to explore it.
If you’re using the Dexcom G5/G6 app as your CGM it only shows the last day’s data, but it uploads data into Dexcom’s servers, and you can use the Dexcom Clarity app on your phone or via the web to explore it.
Medtronic and Abbott (Libre) have similar functionality. xDrip+ has some of this built in, and if you upload your data to your personal Nightscout site there are a lot of analysis tools in Nightscout’s reports. Tidepool and Diasend can also provide insights.
Occasionally actually taking time to look at the data and learn from it can be immensely useful. Not only can you see things like what happened around a particular meal (and for instance make difference choices about insulin timing for the next similar meal) but you can start to see patterns and make changes to eliminate them.
Looking at data from weeks prior when with your doctor usually leads down the “How would I remember what happened?” path. But we can usually remember what happened in the last week. So looking at our own data every now and then is highly recommended.
Closing the loop
Connecting the CGM data into a closed-loop (AID – Automated Insulin Delivery) system is another step. Having a computer make the tiny tweaks for you in the background for all the time you’re not paying attention to your diabetes (and really, who wants to be tied up with diabetes management 24×7?) can be both empowering and result in better health. I think my own amazing results (described in various BionicWookiee updates such as this) provide an example.
We’ve had “DIY” AID systems since 2016, and we now also have two commercial closed-loop systems available in Australia (Tandem’s Control-IQ, and Medtronic’s 780G, along with their earlier 770G/670G).
Of course, an AID system is not a set-and-forget panacea: we still need to review the data (including CGM) from time to time and make tweaks (whether to the configuration or sometimes also to our behaviour).
With CGM more accessible, what will change?
Our behaviour may change, and our options should also change.

Many of us use our CGM systems “off-label”. Sometimes this is by placing them in locations that weren’t approved by the TGA. In fact a range of changes can improve the usability of the systems.
But some of this has been driven by the need for economy in the face of otherwise paying hundreds of dollars EVERY month. There can sometimes be convenience in not having to replace a sensor after exactly 10 (or 7, etc) days. But with lower cost there will be less incentive to try to stretch each sensor out as long as possible.
More CGMs?
With a larger user base (and some people replacing their sensors more often), there may be more financial incentive for CGM providers to enter the Australian market.
Abbott has already retired their original Libre system in favour of the Libre 2 which they brought to Australia last year. Like the original, the Libre 2 wants you to scan every 8 hours to collect the data, but offers phone alarms via Bluetooth. But their Libre 3 (currently being rolled out in more countries) is a full Bluetooth CGM. You only scan it to set it up. It’s physically smaller than the earlier generations too. Work is apparently under way to allow the CamAPS FX AID software to use Libre 3 as well as Dexcom G6.
It’s possible the subsidy may accelerate the eventual introduction of Dexcom’s G7 (which is about to roll out in the US).
There are more CGM companies overseas, and with some interesting products. Mostly these are similar in basic form factor to our current CGM systems. I’ve tried some of them, although I must admit my current preference is for Dexcom.
Part of the financing behind the CGM subsidy is an assumption that NDSS will end up spending less subsidising BG test strips every month. I’m not privy to their financial models, but this is obviously going to have some effect on the BG strip suppliers. Abbott would be hoping that sales of their FreeStyle strips that fall away might be made up by increased Libre traffic. ![]() But not all suppliers also have CGM in their portfolio. It may be relevant that Ascensia (the company behind the Contour Next meters and strips) has the worldwide distribution rights for the implanted Eversense CGM.
But not all suppliers also have CGM in their portfolio. It may be relevant that Ascensia (the company behind the Contour Next meters and strips) has the worldwide distribution rights for the implanted Eversense CGM.
More loops?
Closed-loop (AID) systems may become more widely available. More will presumably be coming, especially as now the main financial barrier to using AID has gone (paying for the CGM, assuming the pump cost is already dealt with).
I’m not saying that everyone can afford a pump at the moment, but up to now CGM use has been more expensive (even without a pump) than NDSS-subsidised pump use.
- Tandem (via AMSL) already provides Control-IQ at no added charge to in-warranty t:slim pump users.
- I would not be surprised if Medtronic rolled out 780G upgrades to all in-warranty pump users. It would be nice if they did that for free: it would certainly drive their CGM business.
- More commercial AID options may open up in Australia too. Especially with pump systems that have been setting up CGM integration already.
Insulet are still working to get their Omnipod DASH pumps subsidised in Australia, but it’s worth noting that they’re currently rolling out their Omnipod 5 AID system (which currently interfaces with Dexcom G6) in the US. - Of course the opensource AID options aren’t standing still either!
How quickly things develop is a little bit of a crystal-ball-gazing exercise, but I expect some of these changes will appear this year.
Conclusion
It was wonderful to see the bipartisan commitments to providing CGM for Australians with T1D! Hopefully it comes true, and hopefully without too many hiccups.
Not only will it save many of us money that we have been spending to stay healthy with this disease (that none of us ever asked for) but it should also change the economics of the Australian T1 scene and open up a string of new options and opportunities for us.
Of course, we will continue to advocate for equitable access for everyone who will benefit from this technology. #CGM4ALL

What a wonderful article David…thank you for putting it all together…
Thank you for this thoughtful article. I’m currently self funding the Freestyle Libre 2 – partly due to cost but also issues with a trial of the Dexcom 4 (years ago) and excessive alarms on that system. I’m not sure I am as brave as you in setting up my own closed loop but hope Ypsomed (my current pump) stick to their promises and implement an officially sanctioned version soon. As I see it, the technology is there but government’s willingness to acknowledge it is still lacking. Subsidised CGM is a big step towards that goal.
Hi David
A very comprehensive article. The ultimate goals of NDSS and indeed the PBS is maximise good health outcomes for patients, and to reduce the drain (resources and financial) on the health system. I strongy believe continuous glucose monitors (CGM)s contribute to these goals
I agree with your comments on educating new CGM users. If there is an initial rush for non-CGMers to take advantage of the subsidised then I’m not sure how these people will learn how to “do it”. There are not enough educaters, the pharmacist may not have the time or skills, people who could benefit from a CGM may just say it’s too hard and revert to their previous methods of BGL control.
I also believe this is an opportunity for the government/NDSS/PBS to challenge the CGM manufacturers to make sure we are getting best of breed systems. My current solution is MDI and Abott Freestyle Libre 1 (FSL1) with a MiaoMiao3 (MM3) and xDrip+ software on phone and watch. It has improved my HbA1c to mid 6s, an outcome with which I am pleased. Abbott have end-of-lifed the FSL1 and introduced the FSL2 with their LibreLink (LL) app. The FSL2/LL is not a CGM solution. Yes, it receives readings every 1-5 minites but the user doesn’t get to see them unless they scan the sensor with a reader. This is a flash glucose monitor (FGM), not a CGM. It’s like an aeroplane without an altimeter, just an alarm when the ground gets too close, but you’re not sure how you got there. Governments/NDSS/PBS should be active in ensuring the systems, not just the sensors, will provide the best solutons for patients.